Long COVID research is making progress
This is an article review of the recently released article entitled Long COVID: major findings, mechanisms and recommendations by Nature.com with contributions by Jon Lesko, covidCAREgroup Research Advisor.
Updated December 28, 2023
Nature.com recently published research about Long COVID which serves as an update on the status of current research, barriers to diagnosis, and treatment, with CCG recommendations on managing Long COVID symptoms and applying for US disability benefits. Here we will break down the key points and add information to make it easier to understand by adding italicized teal notes. The analysis on long COVID by the authors of this paper is quite comprehensive and detailed. It delves into the complexity of the condition and how many different symptoms or potential causes overlap. This becomes critical given that there is no clear definitive cause or treatment. While a significant portion of the document and references focus on ME/CFS it is of great value because of the depth of the analysis. In order to find treatments or cures the research needs to embody as much of the available information as possible.
At the time the article was written, Long COVID was projected to impact 65 million cases worldwide, but according to the Johns Hopkins University COVID-19 tracker, as of January 14, 2023, there were 667 million cases documented worldwide, and 101 million documented cases in the U.S. Using this article’s estimate of a 10% Long COVID frequency, we can project that Long COVID affects at least 67 million people worldwide, and 10 million in the U.S. Other researchers have estimated Long COVID occurrences to affect 30-50% of those exposed to the spike protein in either the virus or vaccine. These numbers do not include undocumented home tests, false negatives, or vaccine side effects.
Excerpts from the article released by Nature Reviews Microbiology on Nature.com:
Biomedical research has made substantial progress in identifying various pathophysiological changes and risk factors and in characterizing the illness; further, similarities with other viral-onset illnesses such as myalgic encephalomyelitis/chronic fatigue syndrome and postural orthostatic tachycardia syndrome have laid the groundwork for research in the field. In this review, the authors explore the current literature and highlight key findings, the overlap with other conditions, the variable onset of symptoms, long COVID in children and the impact of vaccinations. Although these key findings are critical to understanding long COVID, current diagnostic and treatment options are insufficient, and clinical trials must be prioritized that address leading hypotheses. Additionally, to strengthen long COVID research, future studies must account for biases and SARS-CoV-2 testing issues, build on viral-onset research, be inclusive of marginalized populations and meaningfully engage patients throughout the research process.
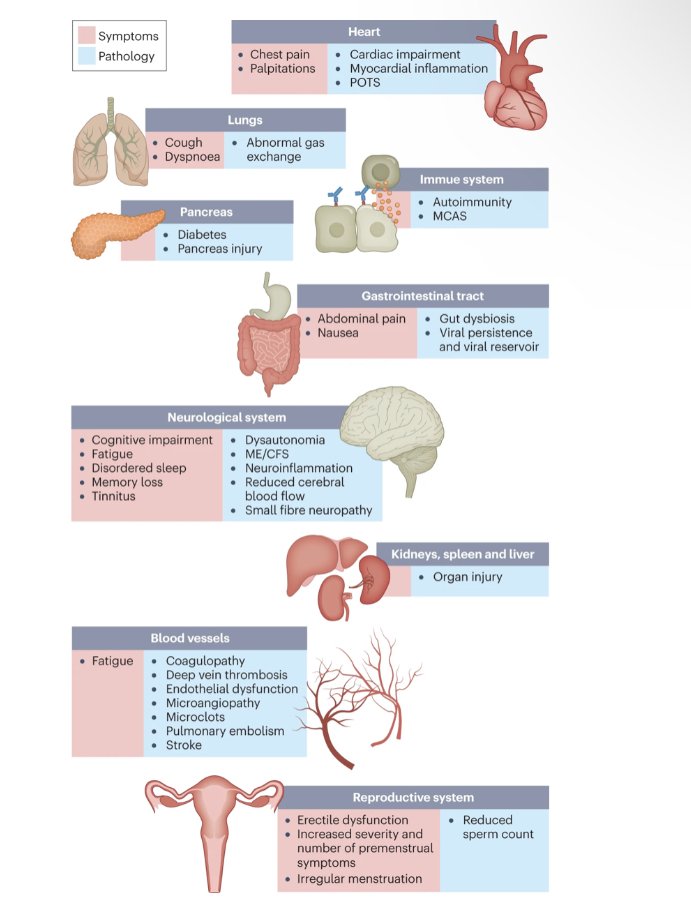
Long COVID is an often debilitating illness that occurs in at least 10% of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections. More than 200 symptoms have been identified with impacts on multiple organ systems.
Long COVID is associated with all ages and acute phase disease severities (meaning you can get Long COVID even if you had a mild case of COVID-19), with the highest percentage of diagnoses between the ages of 36 and 50 years. Most long COVID cases are in non-hospitalized patients with a mild acute illness.
Hundreds of biomedical findings have been documented, with many patients experiencing dozens of symptoms across multiple organ systems. Long COVID encompasses multiple adverse outcomes, with common new-onset conditions including cardiovascular, thrombotic and cerebrovascular disease, type 2 diabetes, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and dysautonomia, especially postural orthostatic tachycardia syndrome (POTS).
Symptoms can last for years, and particularly in cases of new-onset ME/CFS and dysautonomia are expected to be lifelong. With significant proportions of individuals with long COVID unable to return to work, the scale of newly disabled individuals is contributing to labour shortages. There are currently no validated effective treatments.
Here is a diagram depicting the impact of long COVID on numerous organs with a wide variety of pathology. The presentation of pathologies is often overlapping, which can exacerbate management challenges. MCAS, mast cell activation syndrome; ME/CFS, myalgic encephalomyelitis/chronic fatigue syndrome; POTS, postural orthostatic tachycardia syndrome.
Note: In this section, you will see medical terms reworded to make it easier to understand in black italics.
One year after the initial infection, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections increased the risk of cardiac arrest, death, diabetes, heart failure, pulmonary embolism and stroke, as studied with use of US Department of Veterans Affairs databases Additionally, there is clear increased risk of developing myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and dysautonomia. Six months after breakthrough infection, increased risks were observed for cardiovascular conditions, coagulation and hematological conditions, death, fatigue, neurological conditions and pulmonary conditions in the same cohort. -This comment does not tell us the age and general health conditions of the people who developed these complications, so this information may not apply to the general population, but these conditions listed are among the top 5 Long COVID symptoms reported by followers.
There are several hypothesized mechanisms for long COVID pathogenesis, including immune dysregulation, microbiota disruption , autoimmunity , clotting and endothelial abnormality , and dysfunctional neurological signaling . EBV, Epstein–Barr virus; HHV-6, human herpesvirus 6; SARS-CoV-2/severe acute respiratory syndrome coronavirus 2. -Researchers are still working to confirm the cause of the cytokine storm and MCAS that lead to dysautonomia (when the immune system mistakes the organs for invasive germs and tries to eliminate them) and the histamine cascade that causes inflammation. The microbes of the gut that are essential for digestion and nutrient absorption are impacted by Long COVID, and it affects the blood components and blood vessels. The conditions listed are: EBV is mononucleosis..HHV-6 is a herpes virus that typically infects approximately 70% of children by the age of three and often results in fever, diarrhea, sometimes with a rash known as roseola. Human herpesvirus 6 is an uncommon viral infection that usually arises due to the reactivation of the human herpes virus type 6 (HHV-6) in the body, often resulting from a decreased immune system in the adult. and SARS-C0V-2 is COVID-19 or coronavirus.
Although COVID-19 was initially recognized as a respiratory illness, SARS-CoV-2 has capability to damage many organ systems. The damage that has been demonstrated across diverse tissues has predominantly been attributed to immune-mediated response and inflammation, rather than direct infection of cells by the virus. Circulatory system disruption includes endothelial dysfunction and subsequent downstream effects, and increased risks of deep vein thrombosis, pulmonary embolism and bleeding events. Microclots detected in both acute COVID-19 and long COVID contribute to thrombosis. -DVTs are also known as blood clots, and thromboisis is a blood clot that has traveled to the lungs, heart or brain, and embolism is a foreign material that has blocked a blood vessel, commonly caused by fat, cholesterol or vessel wall pieces that have broken loose and entered the blood stream. Microclotting is common in COVID and Long COVID, but this is treatable with medication.
Long-term changes to the size and stiffness of blood cells have also been found in long COVID, with the potential to affect oxygen delivery and are an attractive diagnostic and therapeutic target. A long-lasting reduction in vascular density, specifically affecting small capillaries, was found in patients with long COVID compared with controls, 18 months after infection. -Each healthy red blood cell carries four molecules of oxygen, RBCs are created in the bone marrow in about 120 days, which correlates with the onset and recovery time for a lot of people with long COVID, but some people continue to have issues for 18 or more months post infection.
The widespread lack of knowledge of viral-onset illnesses, especially ME/CFS and dysautonomia, as well as often imperfect coding prevents these conditions from being identified and documented by clinicians; this means that they are frequently absent from electronic health record data. Further, because ME/CFS and dysautonomia research is not widely known or comprehensively taught in medical schools, long COVID research is often not built on past findings and tends to repeat old hypotheses. Additionally, long COVID research studies and medical histories tend to document only the risk factors for severe acute COVID-19, which are different from the risk factors for conditions that overlap with long COVID such as ME/CFS and dysautonomia. -Information and education are needed because there is still so much unknown and COVID-19 doesn’t fit into the previous categories, but doctors may not be aware that there is more to learn.
Clinicians who are not familiar with ME/CFS and dysautonomia often misdiagnose mental health disorders in patients; four in five patients with POTS receive a diagnosis with a psychiatric or psychological condition before receiving a POTS diagnosis, with only 37% continuing to have the psychiatric or psychological diagnosis once they have received their POTS diagnosis. Researchers who are unfamiliar with ME/CFS and dysautonomia often do not know to use specific validated tools when conducting mental health testing, as anxiety scales often include autonomic symptoms such as tachycardia, and depression scales often include symptoms such as fatigue, both of which overestimate mental health disorder prevalence in these conditions. -Our followers report the same, with many women having been involuntarily admitted to psych wards after they reported post COVID shaking, muscle spasms, jaw clenching, crying, irritability, depression, and anxiety, all of which can be traced directly back to inflammation of the brain and central nervous system.
Although research into long COVID has been expansive and has accelerated, the existing research is not enough to improve outcomes for people with long COVID. To ensure an adequate response to the long COVID crisis, we need research that builds on existing knowledge and is inclusive of the patient experience, training and education for the healthcare and research workforce, a public communication campaign, and robust policies and funding to support research and care in long COVID.
Article recommendations: Further and ongoing research into Long COVID and other post viral conditions; the development of physician education; a public communication campaign for the biomedical community and public about the risks and outcomes of Long COVID; and the development of policies and funding that will sustain long COVID research and enable people with Long COVID to receive support.
Conclusions: Long COVID is a multisystemic illness encompassing ME/CFS, dysautonomia, impacts on multiple organ systems, and vascular and clotting abnormalities. It has already debilitated millions of individuals worldwide, and that number is continuing to grow. On the basis of more than 2 years of research on long COVID and decades of research on conditions such as ME/CFS, a significant proportion of individuals with long COVID may have lifelong disabilities if no action is taken. Diagnostic and treatment options are currently insufficient, and many clinical trials are urgently needed to rigorously test treatments that address hypothesized underlying biological mechanisms, including viral persistence, neuroinflammation, excessive blood clotting and autoimmunity.
Read the full scientific article at Nature Reviews Microbiology (Nat Rev Microbiol)ISSN 1740-1534 (online) ISSN 1740-1526.
What does this mean to you?
First and foremost, scientists are advocating for those with Long COVID and for the recognition of the threat it presents to the community while acknowledging the insufficient information and care available.
Key takeaways: The article identifies the damage Long COVID can cause. This is evident in the top 5 symptoms covidCAREgroup followers report: Fatigue, brain fog, insomnia, depression and anxiety. When left unaddressed, people with Long COVID continue to experience progressive damage for at least 6 to 12 months post spike protein exposure. This happens from the disturbance of the immune system that leads to inflammation of nerves, organs and tissues, and by causes autoantibodies (antibodies are protective, autoantibodies damage the body) to attack internal organs and systems. The immune compromise also gives any dormant conditions like EBV (mononucleosis), cancer, HIV, Lyme, varicella (chicken pox, shingles), etc., an opportunity to reactivate and or grow, adding to the challenges of recovery.
People More Likely to Develop Long COVID (CDC)
Some people may be more at risk for developing post-COVID conditions (or long COVID). Researchers are working to understand which people or groups of people are more likely to have post-COVID conditions, and why. Studies have shown that some groups of people may be affected more by post-COVID conditions. These are examples and not a comprehensive list of people or groups who might be more at risk than other groups for developing post-COVID conditions:
People who have experienced more severe COVID-19 illness, especially those who were hospitalized or needed intensive care.
People who had underlying health conditions prior to COVID-19.
People who did not get a COVID-19 vaccine.
People who experience multisystem inflammatory syndrome (MIS) during or after COVID-19 illness.
How can you prevent Long COVID or permanent damage?
Prevention is the best approach!
Prevention through healthy life style and nutrition, social distancing, handwashing, avoiding crowded spaces with poor ventilation and when appropriate, vaccination.
Nasal flushing, gargling, and swishing daily to wash out viral particles.
Early intervention is the key!
If you think you have been infected or re-infected, get tested or do a home test.
If you test positive, ask your doctor about anti-viral medication within the first 5 days of infection.
If you get sick, focus on early intervention and utilize the antihistamine, anti-inflammatory, and anticoagulant protocols as well as other resources that are available.
Keep learning and advocating!
If your doctor doesn’t have answers, keep looking.
Remember western medical doctors are trained in medication and surgery and they may not have all of the answers.
You need to take charge of your recovery through education and self-advocacy.
Consider complimentary alternatives such as Chinese medicine, acupuncture, nutrition, counselling or other types of care if you need extra help.
Medication protocols for long COVID prevention and treatment
Talk to your doctor about the top 4 concerns: Histamines, Inflammation, Depression, and Blood Clotting
The antihistamine protocol: Seasonal allergy medicines like Allegra or Zyrtec (H1 blockers) and antacids like famotidine or Pepcid (H2 blockers) to counter the histamine cascade.
The anti-inflammatory protocol: Such as steroids in severe cases, or NSAIDs like ibuprofen or other prescription medications to reduce inflammation, pain, and the risk of damage to nerves and organs.
The antidepressant protocol: SSRI and SNRI medications to reduce depression, anxiety or fatigue.
The anticoagulant protocol: Aspirin, baby aspirin or prescription medications to prevent micro-clotting or deep vein thromboses (DVT) that can cause neural damage, organ damage, or stroke by blocking the flow of blood to vital organs.
Guidance on “Long COVID” ADA Disability, Section 504, & Section 1557 (CDC)
Barriers to diagnosis and treatment
Some post-COVID conditions cannot be detected with the current diagnostic tools. Clinical evaluations and results of routine blood tests, diagnostic imaging, and electrocardiograms may be normal. Many of the symptoms are similar to those reported by people with ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome) and other poorly understood chronic illnesses that may occur after other viral infections such as Lyme Disease. People with these unexplained symptoms may be misunderstood by healthcare providers, which may result in delayed diagnosis and treatment.
Many people with COVID-19 get better within weeks, some people continue to experience symptoms that can last months after first being infected or may have new or recurring symptoms at a later time. This can happen to anyone who has had COVID-19, even if the initial illness was mild. People with this condition are sometimes called “long-haulers.” This condition is known as “long COVID.”
Qualifying for Social Security Disability
According to JAMA, at least 12% of people have been disabled by the COVID-19 spike protein, regardless of the severity of infection or how they were exposed (virus or vaccine). That number equated to 10.8 million people in the US as of August 1, 2022 based on the 90 million cases of COVID infections on that date. In January 2023 the number of documented US COVID cases passed 101 million, meaning at least 12 million people likely have Long COVID. Other researchers estimate the frequency of Long COVID is closer to 30-50%.
Symptomology that lasts or increases at the 6-month mark indicates a high risk of some level of disability, the benchmark for social security disability (SSD) eligibility. 4 or 5 months of persistent or worsening post COVID sequelae indicates that it is time to consider what is needed to qualify for SSD benefits.
Most social security applications are denied due to lack
of:
Lack of documented evidence of disability
Lack of awareness of Long COVID by providers and patients
Lack of diagnostic testing to confirm Long COVID
Key medical documentation includes:
Confirmation of COVID-19 infection by positive test or documented new onset health issues that started after bing infected or vaccinated
Inflammatory markers and/or COVID-19 antibodies detected in blood work
Diagnostic testing that indicates organ dysfunction (bloodwork, CT, MRI, Ultrasound, etc)
Full neuropsychological evaluation to assess cognitive impairment
Functional capacity exam to assess physical impairment
Steps 4 & 5 are especially helpful in providing that documentation if you are denied on the first SSD application. This approach should work even if you do not have a specific diagnosis of Long COVID by identifying your specific limitations.
It’s also important to keep in mind that over the next few years, you may recover to the point of being able to return to work.
Testing may identify a treatable condition, inflammation may resolve, etc.
You may find a new career that allows you to work within your limitations.
The process of applying for disability benefits of any type is complicated.
ProMedView Clinical Consultants can guide you through the process of obtaining sufficient documentation for your SSD application.
The U.S. Department of Health and Human Services and the Department of Justice jointly published a guidance document on “long COVID” as a disability under the Americans with Disabilities Act (ADA), Section 504 of the Rehabilitation Act, and Section 1557 of the Affordable Care Act. The guidance, released as we commemorate the 31st anniversary of the ADA, provides additional clarity on how these disability nondiscrimination laws apply to people who may be newly covered under these laws because of the impact of the COVID-19 infection on their bodies and their lives. The document discusses when long COVID may be considered a disability under the ADA, Section 504, and Section 1557, and shares examples along with related resources that may be helpful. Read the Guidance (July 2021).
The United States civil rights protections and responsibilities of these federal laws apply even during emergencies. They cannot be waived. Follow this link for more information: If you are in the U.S. and need information on filing for disability with information about getting your disability documented, read this covidCAREgroup article: New guidance released regarding Long COVID as a Disability — covidCAREgroup
The future may look different than it did before the pandemic, but we are resilient, and we can choose not to be defined by Long COVID because we are capable of adapting to new challenges.
With lifestyle changes and time to recover, many of us have the ability to get stronger and back on our feet. It’s better for you and the community if you are living as close to a normal life as possible including family, home, work, and social activities.
You can stop or modify SSD benefits at any time when you and your body are ready. Do your best to stay focused on recovery and management of Long COVID and try to avoid the “disabled” or “sick” mindset.
Things you can do to help yourself
Minimizing physical & psychological stressors is essential in recovery from Long COVID.
Nutrition: Try to eat protein and fresh vitamin rich foods daily and avoid chemicals, preservatives, sugars, fast foods, prepared foods and high histamine foods.
Don’t skip meals. Your body needs protein , vitamin C, and vitamin D to heal from any injury or illness. A low histamine or low carbohydrate (sugar) diet is recommended by doctors treating Long COVID (PASC), and many people report a reduction in symptoms within 1-3 days of the diet change, including decreases in sneezing, itching or hives, irritable bowel syndrome, body pain, along with a reduction in swelling and inflammation.Hydration: A minimum of eight 8 oz glasses of plain water daily is recommended.
Avoid drinks with chemical additives. You can easily make a fresh electrolyte drink yourself by adding a dash of mineral rich Epsom salt and a piece a fruit like a raspberry for flavor instead of spending money on commercial drinks like Gatorade that contain chemicals and sit in plastic bottles for long periods of time. Remember that caffeine and alcohol have dehydrating effects.Sleep hygiene: Getting 7-9 hours of sleep so your body can repair itself. You need at least 4 hours of uninterrupted sleep to get into the restorative phase of sleep.
Avoid stimulating activities after dinner like thrilling movies or books, arguments, negative news or frustrating stimuli.
If you wake up frequently or with a startle, you may be experiencing drops in your oxygen level, which signal your brain to release adrenaline to force you to take a breath. This could be a temporary inflammation issue or more enduring sleep apnea. Ask your doctor for a sleep study to evaluate your need for a CPAP or BiPAP, a machine that pushes air into your lungs when it senses an apneic episode (periods of not breathing).Stress management: Stress affects every component of your life.
The only thing you can control about stress is your reaction to it. Try to avoid or minimize your exposure to stressful situations: Turn off the news, make family visits that end unpleasantly short, wait for the morning to have intense discussions, let go of things that annoy you but don’t really matter in the big scheme of things, avoid intense conversations or entertainment in the evening.
Exercise within tolerance: Pace yourself and do not push your body to extremes in any way.
For some this may mean seated breathing exercises, walking to the mailbox. Rest when your body says to slow down. Gradually build on your activity endurance as your body cues you to progress. This can be hard to gauge, because when you feel good you naturally do more, but if you do too much you may experience symptom flare ups 1-3 days later as the post exertion inflammation builds. Some people describe this as post exertional malaise, others experience severe recovery set backs.
Breathwork: You can literally stop the fight or flight reaction by taking slow deep breaths.
Deep slow breathing shuts down the adrenaline flow, slows your heart rate, lowers your blood pressure and decreases stress related histamine release. When you do this, your blood reroutes back to your brain and nervous system to allow you to think clearly. It also allows your body to use its energy and oxygen to heal your inflamed nerves and organs.
Keep moving, keep breathing.
Brought to you by covidCAREgroup, connecting the dots of long COVID through education, research and resources.
Did this article help you? Please consider making a gift, donating, or purchasing a $25 annual membership. The covidCAREgroup is run by volunteers. 100% of our funding comes from community donations are used to support our continued outreach initiatives.
COVID Care Group, LLC, is not a “not for profit” organization. Donations, gifts & memberships are not tax-deductible.
COVID Care Group, LLC is not a healthcare provider and does not provide medical advice, diagnosis, or treatment.
Resources from covidCAREgroup
Recovery Tools — covidCAREgroup
Education Blog Table of Contents — covidCAREgroup
Long COVID Recovery Information and Resources — covidCAREgroup
Long COVID FAQ — covidCAREgroup
COVID-19 Long Haulers Support Group (Facebook)
Article resources
Nature Reviews Microbiology (Nat Rev Microbiol)ISSN 1740-1534 (online) ISSN 1740-1526
John Hopkins University COVID-19 Tracker
NIH 2017: MERS, SARS and other coronaviruses as causes of pneumonia
CDC Evidence for Limited Early Spread of COVID-19 Within the United States
Outcomes of SARS-CoV-2 Reinfection | Research Square
Long COVID or Post-COVID Conditions
NIH - COVID-19 was third leading cause of death in the United States in both 2020 and 2021
COVID-19 a leading cause of death in US, topped only by heart disease and cancerCenters for Disease Control and Prevention (CDC) - Long-Term Effects of COVID-19
CDC - COVID-19 Vaccination FAQCenters for Disease Control and Prevention (CDC) - Long-Term Effects of COVID-19
CDC - COVID-19 Vaccination FAQ
10 Alternative Medicines Explained
https://www.nccih.nih.gov/health/complementary-alternative-or-integrative-health-whats-in-a-name
Original publication date: January 16, 2023