Is my COVID test positive?
As COVID-19 continues to mutate and spread, many of us find ourselves repeatedly re-testing at home, but are unsure of what a positive test looks like. Any trace of a line is considered positive. This article explains how to do a home test properly and has pictures of actual positive home tests to help you figure this out.
Updated January 7, 2025
What does a positive home test look like?
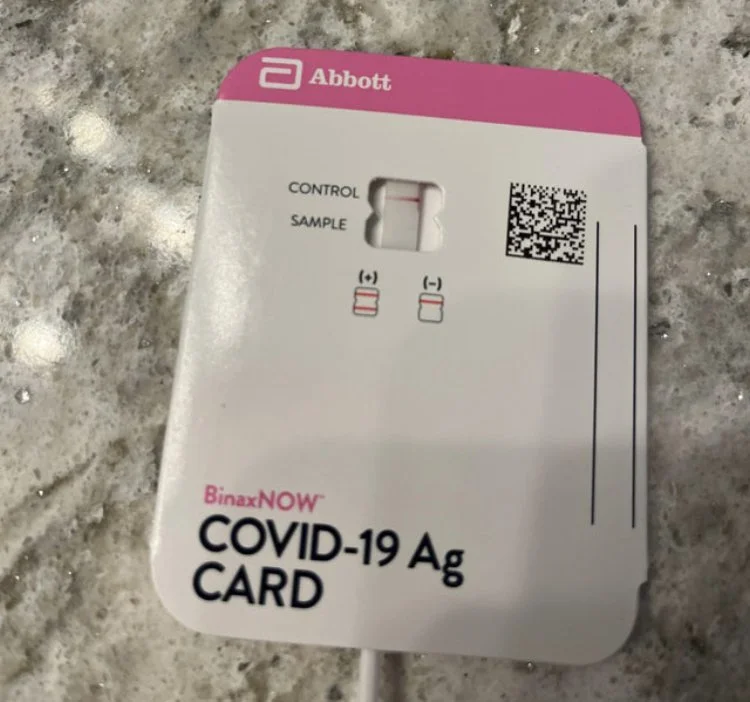
Any trace of the second line is positive. There should be photos with examples in the test package insert. Look for what seems to be a line, regardless of the color. We also have examples from group members below to reference.
This may be difficult for people with slight or severe vision issues or color blindness.
Some people with post COVID hypoxic damage to the eyes have lost the ability to see some reds, along with blurred vision, floaters, blind spots, prism vision, and waterfall vision.
And while you may have had perfect color vision all of your life, there is a chance that it has caused hypoxic damage to your eyes and optic nerve due to a lack of oxygen during the acute infection or post COVID issues. (Read more about COVID Eye Damage)
What should I do if I’m positive?
Isolate yourself.
Talk to your doctor about early intervention with antivirals, antihistamines, anticoagulants and anti-inflammatory protocols. Note: Antivirals need to be started within 5 days of symptom onset. There are some people that “rebound” after finishing the antiviral, but that is most likely the virus running the rest of it’s 10-14 day course. The antivirals are still effective in inhibiting the viral replication while you take them.
The FDA authorized Paxlovid for people ages 12 and older who weigh at least 88 pounds. But in order to qualify for a prescription, you must also have had a positive COVID-19 test result and be at high risk for developing severe COVID-19.
Have household members and others you have been in close contact for 15 minutes or longer in the last 5 days test themselves. Note: According to test package inserts, the test is unlikely to show a positive result during the 3-5 incubation period, others may not test positive 5-8 days.
CDC guidance: When to Consider Taking an At-Home COVID-19 Test
If you have COVID-19 symptoms, test yourself immediately.
If you were exposed to someone with COVID-19, test yourself at least 5 days after your exposure. If you test negative for COVID-19, consider testing again 1 to 2 days after your first test.
If you are going to an indoor event or a gathering, test yourself immediately before or as close to the time of the event as possible. This is especially important before gathering with individuals at risk of severe disease, older adults, or those who are immunocompromised.
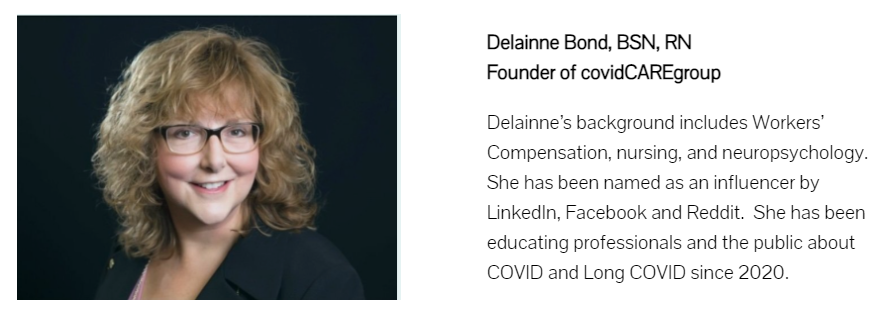
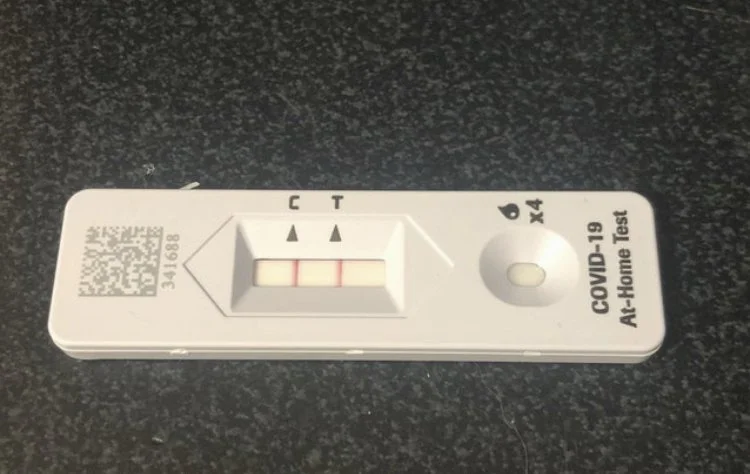
Examples of positive COVID-19 home tests
FDA testing recommendations
The FDA recommends repeat testing following a negative result whether or not you have COVID-19 symptoms.
At-home COVID-19 antigen tests detect proteins, called antigens, from the SARS-CoV-2, the virus that causes COVID-19. At-home COVID-19 antigen tests are less likely to detect the SARS-CoV-2 virus than molecular tests, such as polymerase chain reaction (PCR) tests. This is especially true early in an infection or in people who do not have COVID-19 symptoms. Currently, all at-home COVID-19 antigen tests are FDA-authorized for repeat use. This means people should use multiple tests over a certain time period, such as 2-3 days, especially when the people using the tests don't have COVID-19 symptoms. Today, the FDA is highlighting the continued need for repeat testing when people get a negative result with an at-home COVID-19 antigen test, including recommending additional testing over a longer period of time.
Today's recommendations are based on the latest study results from people with likely omicron infection showing that repeat testing after a negative at-home COVID-19 antigen test result increases the chance of an accurate result.
Before you use a COVID-19 antigen test
Be aware that at-home COVID-19 antigen tests are less accurate than molecular tests. COVID-19 antigen tests may not detect the SARS-CoV-2 virus early in an infection, meaning testing soon after you were exposed to someone with COVID-19 could lead to a false-negative result, especially if you don't have symptoms. This is the reason why repeat testing is important.
If you plan to use at-home COVID-19 antigen tests, have several tests on hand so you can test more than once. You do not need to use the same brand of test each time for repeat testing. Visit At-Home OTC COVID-19 Diagnostic Tests for a list of all FDA-authorized home tests and for more information about who can use a test and for what ages.
Be aware the FDA expects similar performance with Point of Care (POC) COVID-19 antigen tests performed at a clinic or doctor's office. A negative POC COVID-19 antigen test result should also be followed up with repeat testing and an at-home test could be used.
At-home COVID-19 antigen test
If you receive a positive result initially or after a repeat test, this means the test detected the SARS-CoV-2 virus and you most likely have COVID-19.
Follow the Centers for Disease Control and Prevention (CDC) guidance for people with COVID-19, including to stay home, isolate from others, and seek follow-up care with a health care provider to determine the next steps.
If you receive a negative result, the test did not detect the SARS-CoV-2 virus at the time of that test.
If you have COVID-19 symptoms, test again 48 hours after the first negative test, for a total of at least two tests.
If you get a negative result on the second test and you are concerned that you could have COVID-19, you may choose to test again 48 hours after the second test, consider getting a laboratory molecular-based test, or call your health care provider.
If you do not have COVID-19 symptoms and believe you have been exposed to COVID-19, test again 48 hours after the first negative test, then 48 hours after the second negative test, for a total of at least three tests.
If you get a negative result on the second test, test again 48 hours after the second test.
If you get a negative result on the third test and you are concerned that you could have COVID-19, you may choose to test again using an antigen test, consider getting a laboratory molecular-based test, or call your health care provider.
If you get a positive result on any repeat test with an at-home COVID-19 antigen test, you most likely have COVID-19 and should follow the CDC guidance for people with COVID-19.
Things you can do to help yourself
Nutrition: Try to eat protein and vitamin rich foods daily.
Avoid chemicals, preservatives, sugars, fast foods, prepared foods and high histamine foods. Don’t skip meals. Your body needs protein , vitamin C, and vitamin D to heal from any injury or illness. A low histamine or low carbohydrate (sugar) diet is recommended by doctors treating Long COVID (PASC), and many people report a reduction in symptoms within 1-3 days of the diet change, including decreases in sneezing, itching or hives, irritable bowel syndrome, body pain, along with a reduction in swelling and inflammation.
Hydration: A minimum of eight 8 oz glasses of plain water daily is recommended.
Avoid drinks with chemical additives. You can easily make a fresh electrolyte drink yourself by adding a dash of mineral rich Epsom salt and a piece a fruit like a raspberry for flavor instead of spending money on commercial drinks like Gatorade that contain chemicals and sit in plastic bottles for long periods of time.Sleep hygiene: Getting 7-9 hours of sleep so your body can repair itself. You need at least 4 hours of uninterrupted sleep to get into the restorative phase of sleep.
Avoid stimulating activities after dinner like thrilling movies or books, arguments, negative news or frustrating stimuli.
If you wake up frequently or with a startle, you may be experiencing drops in your oxygen level, which signal your brain to release adrenaline to force you to take a breath. This could be a temporary inflammation issue or more enduring sleep apnea. Ask your doctor for a sleep study to evaluate your need for a CPAP or BiPAP, a machine that forced air into your lungs when it senses an apneic episode.Stress management: Stress affects every component of your life.
The only thing you can control about stress is your reaction to it. Try to avoid or minimize your exposure to stressful situations: Turn off the news, make family visits that end unpleasantly short, wait for the morning to have intense discussions, let go of things that annoy you but don’t really matter in the big scheme of things, avoid intense conversations or entertainment in the evening.
Exercise within tolerance: Pace yourself and do not push your body to extremes in any way.
For some this may mean seated breathing exercises, walking to the mailbox. Rest when your body says to slow down. Gradually build on your activity endurance as your body cues you to progress.
Breathwork: You can literally stop the fight or flight reaction by taking slow deep breaths.
Deep slow breathing shuts down the adrenaline flow, slows your heart rate, lowers your blood pressure and decreases stress related histamine release. When you do this, your blood reroutes back to your brain and nervous system to allow you to think clearly. It also allows your body to use its energy and oxygen to heal your inflamed nerves and organs.
Long COVID Solutions
ProMedView Nurse Coaches - We get it.
Our clinical experts advocate for those with Long COVID.
Individual coaching
Group Q&A sessions
Peer support groups
Educational webinars
Keep moving, keep breathing!
COVID Care Group, LLC is not a healthcare provider and does not provide medical advice, diagnosis, or treatment.
Article Resources
CDC: Self-Testing for doing rapid COVID-19 tests anywhere
Scripps: Should I Take Paxlovid if I Get COVID-19?
Yale Medicine: 13 Things To Know About Paxlovid, the Latest COVID-19 Pill
Los Angeles County PAXLOVID FAQs
Original publication date: August 4, 2022